Medical Technologies

Trends in STI Diagnostics
In vitro diagnostics (IVD) play an important role in public health. Efficient and precise tests can facilitate timely and cost-effective treatments, which in turn may reduce the transmission of diseases such as sexually transmitted infections (STIs). STIs are a public health concern, with an estimated 374 million people becoming infected with one of four STIs: Treponema pallidum (syphilis), Chlamydia trachomatis, Neisseria gonorrhoeae and Trichomonas vaginalis.[1] More than one in seven women are estimated to have a human papillomavirus (HPV) infection, the major cause of cervical cancer.[1] In addition, approximately 570,000 new cases of HPV-related cervical cancer were reported in 2018, while in 2019, approximately 300,000 individuals died of HPV-related cervical cancer.[1] Other STIs of concern include the herpes simplex virus (HSV) type 1 (HSV-1), HSV type 2 (HSV-2) and Mycoplasma genitalium. The World Health Organization (WHO) estimates 3.7 billion people under the age of 50 (i.e., 67%) have HSV-1 infection, while approximately 491 million people aged 15-49 (13%) have HSV-2 infection, the cause of genital herpes, globally.[2] As for M. genitalium , an STI that is not widely researched, little to no data is available regarding its population incidence and prevalence, although the Centers for Disease Control (CDC) called M. genitalium an “emerging issue” in its 2015 Guidelines for STIs.[3] In its 2021 Guidelines for STIs, the CDC indicated that M. genitalium is associated with symptoms of urethritis, urethral inflammation, cervicitis, pelvic inflammatory disease and infertility among women. [4], [5]
STI Diagnosis: POC Testing Discovery and COVID-19 Parallels
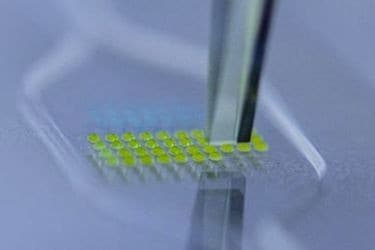
Historically, STIs were identified through phenotypic, culture-based methods. However, recent advancements in immunological and molecular methods have permitted non-phenotypic identification of STIs on large commercial IVD platforms in high-throughput clinical laboratories as well as devices with a smaller footprint that is more appropriate for point of care (POC) environments.[1] The Clinical Laboratory Improvement Amendments (CLIA)-waived POC tests are important for the molecular diagnosis of STIs in not only symptomatic patients but also asymptomatic patients, because CLIA-waived POC tests reduce turnaround times, thereby increasing certainty at the point of need and decreasing the risk of exacerbating antimicrobial resistance in symptomatic patients.[7] Additionally, the availability of high-performing CLIA-waived POC tests could potentially interrupt the transmission of STIs by permitting rapid sexual health screening and help with the prevention of sequelae by diagnosing and treating asymptomatic women under 25 years old, the typical reservoirs of infection.[7] Due to developments in molecular innovation, miniaturization and microfluidics, there are now FDA-cleared tests identified for use at or near POC for STIs, including a wide range of rapid diagnostic tests (RDTs) and simple molecular tests with disposable assays and a small device footprint.[6] [8]
Interestingly, although some lateral flow or RDTs intended for use at or near POC have less than outstanding performances (i.e. high specificity and low sensitivity for analytes such as Chlamydia trachomatis and Neisseria gonorrhoea) [6], a modelling study showed a hypothetical test with a sensitivity ~10% less than currently available reference tests could still have a substantial impact on chlamydia prevalence and pelvic inflammatory disease incidence if over 60% of the screened individuals received immediate treatment. [9] For screened individuals to receive immediate treatment at or near POC, it’s estimated that STI diagnostic assays will have to be less than 20 minutes for results and treatment to occur during a single clinical visit.[7] The amount of time a patient is willing to wait may vary by country and the duration of the test, however. For example, in China, 99% (1484/1497) of patients were willing to wait up to two hours for a test result[10], while in the US, despite an average clinical visit lasting approximately one to two hours, 61% were willing to wait 20 minutes, while only 26% were willing to wait 40 minutes (if they could be treated before leaving the clinic).[11] For a 30-minute test, 89.4% of patients were willing to wait at least 20 minutes after a clinical visit was complete[iv], but for a 90-minute assay, only 21.4% of the patients stayed to receive their results.[13] Therefore, turnaround times, along with cost and sensitivity are important factors to consider when developing or selecting an STI diagnostic for an at or near-POC testing program.
Since the beginning of the COVID-19 pandemic, there’s been an unprecedented emphasis on rapidly increasing the number of diagnostic tests available for detecting SARS-CoV-2. As of September 23, 2021, there were eight Emergency Use Authorized, CLIA-waived molecular diagnostic tests with turnaround times between 11 minutes and 45 minutes, three multiplexed with other respiratory pathogens.[7] Three of these tests have since been FDA-cleared for POC use: the Abbott ID NOW™ COVID-19 2.0 test, the BioFire®COVID-19 Test and the Cue™ [SL3] [DT4] COVID-19 Molecular Test. In addition, there were 15 Emergency Use Authorized, CLIA-waived antigen or lateral flow diagnostic tests available for use, five being over-the-counter (OTC), with turnaround times between 10 minutes and 40 minutes and reasonably high sensitivity in symptomatic patients.[7] Of these tests, only the Quidel® Sofia® SARS Antigen FIA assay has received FDA market clearance at the time this blog was written.
Many molecular assays can be engineered for other targets, increasing the number of STI diagnostic assays available with fast turnaround times and comparable sensitivities.[7] Assays that run on platforms with multiplex capabilities are also suited for the identification of antimicrobial-resistant (AMR) STIs. For example, a multiplex assay that targets the gyrA or parC genes for ciprofloxacin resistance could potentially curb the spread of ciprofloxacin-resistant N. gonorrhoea in locations such as the US, where only a proportion of isolates are resistant to ciprofloxacin.[14]
The integration of more OTC STI tests into the market could further enhance the STI diagnostic framework. While the OraQuick[SL1] [DT2] ® In-Home HIV Test kit remains the only FDA-approved OTC test, the presence of numerous mail-in home test collection kits indicates a clear demand for such products. However, the delay in obtaining results from mail-in tests remains a notable disadvantage. Over-the-counter STI tests can help mitigate this issue by providing immediate results, providing patient confidentiality, and facilitating prompt self-diagnosis and isolation. In doing so, they can potentially serve as a powerful tool in reducing the incidence and transmission of STIs, marking a significant step forward in public health strategies. Furthermore, the desire for OTC STI tests due to the stigma surrounding STIs and their high incidence, makes them an excellent target for IVD development, manufacturing, and marketing.
Citations
[1] Geneva: World Health Organization. (2021) Global progress report on HIV, viral hepatitis and sexually transmitted infections, 2021: Accountability for the global health sector strategies 2016–2021: actions for impact. https://iris.who.int/handle/10665/341412. Accessed 28 November 2023.
[2] Geneva: World Health Organization. (2023) Herpes simplex virus. https://www.who.int/news-room/fact-sheets/detail/herpes-simplex-virus.
Accessed 28 November 2023.
[3] Workowski KA, Bolan GA, Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep. 2015;64(RR-03):1–137.
[4] Sexually transmitted infections treatment guidelines, 2021. Atlanta (GA): Centers for Disease Control and Prevention; 2021. https://www.cdc.gov/std/treatment-guidelines/toc.htm. Accessed 28 November 2023.
[5] Getman D, Jiang A, O’Donnell M, Cohen S. Mycoplasma genitalium prevalence, coinfection, and macrolide antibiotic resistance frequency in a multicenter clinical study cohort in the United States. J Clin Microbiol. 2016;54(9):2278–83. DOI: 10.1128/JCM.01053-16.
[6] Geneva: World Health Organization. (2023) The diagnostics landscape for sexually transmitted infections. https://www.who.int/publications/i/item/9789240077126. Accessed 28 November 2023.
[7] Manabe Y.C. (2023) The impact of the COVID-19 pandemic on technologic and process innovation in point-of-care diagnostics for sexually transmitted infections. Clinical Biochemistry 117:75-83. DOI: 10.1016/j.clinbiochem.2021.11.003.
[8] Peeling RW. Applying new technologies for diagnosing sexually transmitted infections in resource-poor settings. Sex Transm Infect. (2011) 87(Suppl 2): ii28–30. DOI: 10.1136/sti.2010.047647.
[9] Minttu M Rönn, Nicolas A Menzies, Thomas L Gift, Harrell W Chesson, Tom A Trikalinos, Meghan Bellerose, Yelena Malyuta, Andrés Berruti, Charlotte A Gaydos, Katherine K Hsu, Joshua A Salomon. Potential for Point-of-Care Tests to Reduce Chlamydia-associated Burden in the United States: A Mathematical Modeling Analysis, Clinical Infectious Diseases, Volume 70, Issue 9, 1 May 2020,
Pages 1816-1823. DOI: 10.1093/cid/ciz519.
[10] Yin Y, Peeling RW, Chen X, et al. Clinic-based evaluation of Clearview Chlamydia MF for detection of Chlamydia trachomatis in vaginal and cervical specimens from women at high risk in China. Sexually Transmitted Infections. (2006) 82: v33-v37.
[11] Widdice, Lea E., Hsieh, Yu-Hsiang PhD†; Silver, Barbara BS, MBA†; Barnes, Mathilda MS†; Barnes, Perry MSPM†; Gaydos, Charlotte A. MS, MPH, DrPH†. Performance of the Atlas Genetics Rapid Test for Chlamydia trachomatis and Women's Attitudes Toward Point-Of-Care Testing. Sexually Transmitted Diseases 45(11): p 723-727, November 2018. | DOI: 10.1097/OLQ.0000000000000865
[12] Gettinger, Jesse BS; Van Wagoner, Nicholas MD; Daniels, Brice; Boutwell, Alexander MS; Van Der Pol, Barbara PhD, MPH. Patients Are Willing to Wait for Rapid Sexually Transmitted Infection Results in a University Student Health Clinic. Sexually Transmitted Diseases 47(1): pp. 67-69, January 2020. | DOI: 10.1097/OLQ.0000000000001083
[13] Harding-Esch EM, Nori AV, Hegazi A, et al. Impact of deploying multiple point-of-care tests with a ‘sample first’ approach on a sexual health clinical care pathway. A service evaluation. Sexually Transmitted Infections. 2017. 93: 424-429.
[14] Melendez J.H., Hardick J., Barnes M., Page K.R., Gaydos C.A., Antimicrobial
Susceptibility of Neisseria gonorrhoeae Isolates in Baltimore, Maryland, 2016:
The Importance of Sentinel Surveillance in the Era of Multi-Drug-Resistant
Gonorrhea, Antibiotics (Basel) 7(3) (2018).