White Paper
Sleep Apnea and Sleep Study Equipment
Learn how sensors play a vital role in sleep monitoring, the fastest growing segment of the IoMT (Internet of Medical Things).
INTRODUCTION
One of the most talked about topics today is the Internet of Things, or IoT, and how it will transform how we work, how we play, how we relax and much more. While the term IoT can refer to connected products, more specific terms are becoming more common such as the IIoT (Industrial Internet of Things) and IoMT (Internet of Medical Things).

From a medical perspective, IoT-connected devices are being developed for a wide range of applications that include diagnostic and treatment applications as well as monitoring
applications. IoMT devices can provide real-time, continuous information to a central
point that allows doctors and other medical technicians to remotely gather a wide range
of diagnostic and clinical information about their patients safely and securely. Analyzing
this information automatically and/or by a medical professional can help determine medical needs or, for patients with known conditions, it can allow them to be monitored in a home setting that can drastically reduce the cost of monitoring. This allows patients more time at home in a more comfortable setting while increasing space for other patients at hospitals or other medical facilities.
Remote healthcare monitoring is even more important when people are unwilling or unable to provide their own health data – such as when they are asleep. A recent report found that sleep monitoring and sleep therapy is the fastest growing segment of the IoMT healthcare market, and the number of sleep therapy patients has more than doubled in recent years.

Sleep Monitoring Devices
These can be an effective and affordable option to monitor a person’s sleeping patterns.
They can monitor a person’s sleep cycles and track unusual events that could be used to
diagnose sleep apnea as well as a range of other health issues. Health care professionals
can use this information to make informed decisions about a patient’s treatment. Sleep
therapy devices can be used to control and treat a range of sleep disorders and there
are IoMT devices that may moderate snoring, if not actually cure it. Advances in sensor
technology and connectivity have allowed for a range of developments in the diagnosis and
treatment of common sleeping disorders.
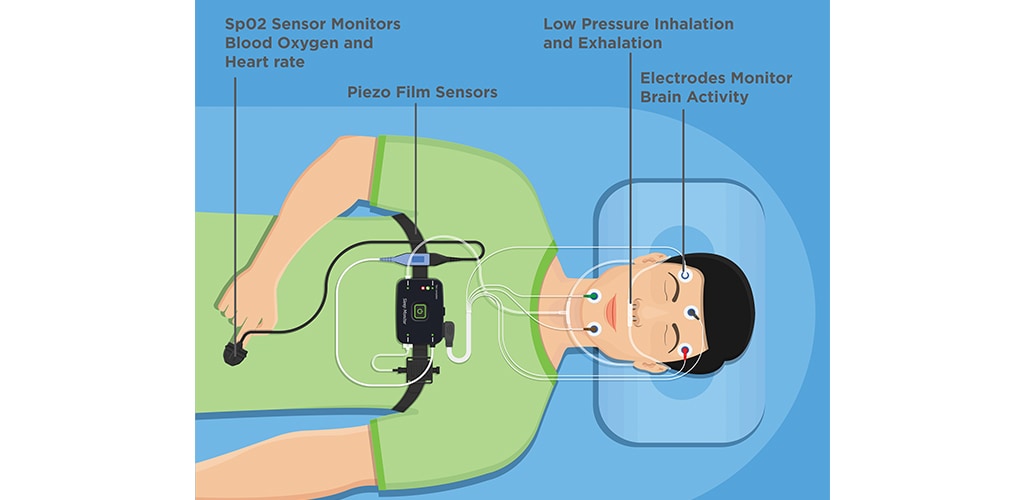
FIGURE 1. SENSING TECHNOLOGIES THAT ARE USED TO DIAGNOSE AND TREAT SLEEP DISORDERS

Sleep Studies
In the past, sleep studies required a visit to a hospital or a sleep center where a patient would be monitored for one or more nights to track a range of data including:
- heart and breathing rate
- blood oxygenation
- amount of overall sleep
- amount of deep sleep
- instances of snoring
- stopped breathing events
There were several issues with clinical sleep studies including high costs, the unwillingness of many people to go to the clinics and the overall validity of data collected in a clinical setting versus a normal home setting. In the past several years, sleep studies have migrated from a clinical setting to a home setting which solved a few problems but made the collection of sleep data more difficult.
Home sleep study systems have been developed to allow the continuous monitoring of heart rate, breathing rate, blood oxygen levels, stopped breathing events along with more sophisticated systems that can also monitor sleep position as well as room temperature and humidity and more. These systems either stream the data continuously to the cloud where the data can be stored or store all the data on memory that is internal to the system. Data that is collected can then be analyzed either automatically and/or by a health professional to determine the type and severity of the sleep disorder

Sleep Monitoring Systems
Sleep monitoring systems generally consist of an array of sensors that can monitor physiological parameters, such as heart and breathing rate, and environmental conditions, such as temperature and humidity. Sensors that can determine other sleep or breathing-related variables such as body movements, blood oxygen levels and air flow measurement can also be included. The range of sensors can include the following:
- Piezo-film sleep sensor with sleep monitoring function to monitor respiratory rate, heart rate, physical activity, deep sleep, light sleep and more
- Photo optic SpO2 sensors to non-invasively measure blood oxygenation
- Low pressure airflow sensors to measure pressures during inhalation and exhalation
- Humidity and temperature sensors to measure intake and exhaust air temperature and humidity
Following the diagnosis of the sleeping issue a treatment plan can be developed that can include a range of equipment, diet, exercise and often, the monitoring of sleep patterns and other physiological data.
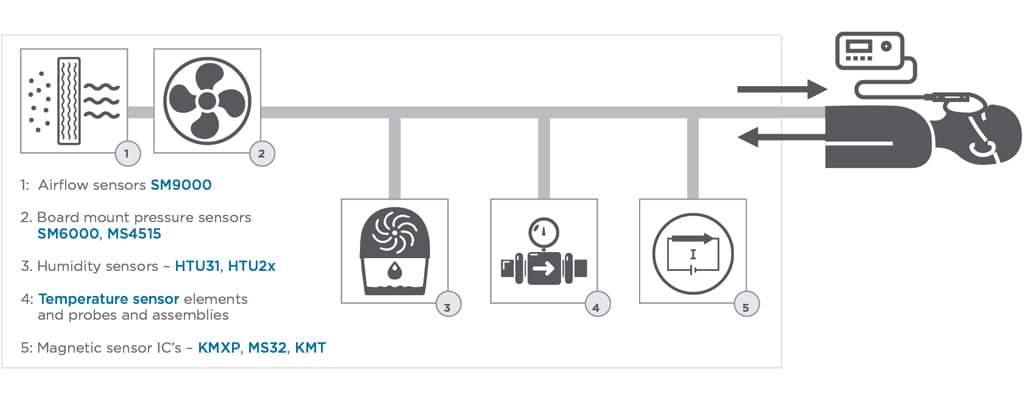
FIGURE 2. SLEEP APNEA MACHINES FEATURING TE CONNECTIVITY’S SENSOR PRODUCTS

Sleep Apnea
The most common sleep disorder is sleep apnea which is a serious disorder where a patient’s breathing repeatedly stops and starts. Patients with sleep apnea will sometimes snore loudly and often will feel tired even after a full night’s sleep.
There are three main types of sleep apnea:
- Obstructive sleep apnea, the mostcommon form that occurs when the throat muscles relax
- Central sleep apnea, which occurs when the brain does not send proper signals to the muscles to control breathing
- Complex sleep apnea syndrome, which occurs when someone has both obstructive sleep apnea and central apnea
Awareness and the simplicity of usage has increased the popularity of sleep apnea machines. Soft tissues around the throat, tongue and palate can collapse on some people during deep sleep. This will partially block the breathing passage resulting in snoring. Snoring can be minimized by keeping the trachea open by applying a small amount of positive air pressure. That is what the sleep apnea machines are designed to do.

Positive Air Pressure (PAP) Machines
There are three main types of positive air pressure (PAP) machines that are used to treat the condition – CPAP, AutoCPAP and BiLevel devices. All of these devices control the flow of air to the patient but do so in different ways with increasing complexity and cost.
CPAP stands for Continuous Positive Airway Pressure and these devices provide a constant and continuous flow of air that the patient must inhale and then exhale. This is the most basic PAP device and is most often prescribed first. In many cases insurance coverage will dictate CPAP first, because it costs less and most patients do well with it. One of the biggest challenges adjusting to CPAP is the overwhelming feeling of that continuous flow of air pressure upon exhalation. Most manufactures offer a resolution to this challenge by sensing and / or reducing the machine pressure upon exhalation.
AutoCPAP – Automatic continuous positive airway pressure (or APAP). Unlike CPAP which is set to deliver one continuous pressure, APAP is set within a high and low-pressure range for the purpose of varying inhalation needs. The range is usually predetermined, and these devices have a sensitive algorithm technology that allows the machine to detect how much inhalation pressure is needed with each breath. The theory of providing a range is that one’s pressure needs may vary during any given night or hour of sleep. Factors that could affect inhalation pressure include sleeping position, cold or allergies, alcohol consumption and medications.
BiLevel indicates a PAP device that delivers 2 distinct pressures, one for inhalation and the second for exhalation. With it being the most complex device, it is also the most expensive and typically reserved for special needs. Since BiLevel works similarly to a ventilator, it is commonly used for patients with other disorders such as ALS, Parkinson’s or other diseases with patients who need assistance with breathing. It is also frequently prescribed for patients who have central sleep apnea, although many with central apnea do quite well with CPAP or APAP.
A basic PAP machine will generally consist of a fan or motor to provide pressurized air, a mask to deliver the air and some type of control display. More sophisticated systems will add additional features and controls. The patient wears a mask that uses pressure to send air flowing through the nasal passages so that they do not collapse and cause breathing to cease. A range of sensors are typically used to monitor and control air pressure as well as to monitor the environment and other aspects of the equipment. We manufacture many sensors that may be used in sleep apnea machines. They are designed to help monitor and control air flow, air pressure, temperature and humidity and provide feedback for motors, fans and blowers.
When low pressure air is forced continuously into a sleep apnea equipment breathing mask to keep the trachea open, the addition of warm, moist air can significantly enhance the comfort level of the patient. Several newer sleep apnea machines are equipped with this option. Moisture in the airstream must be monitored and controlled and TE offers specific sensors to measure and regulate humidity, temperature and other parameters.

Sensors, like electronics in general, continue to evolve with smaller footprints, better
accuracy, fully digital outputs and lower power. Low power operation allows them to be used
in a wider range of applications including battery powered systems. Smaller footprints
allow the sensors to be located closer to the breathing mask and allows for measurement
and control right at the location of interest.

TE has introduced the HTU31 surface mountable humidity/temperature digital output combo sensor in a 2.5 x 2.5 x 0.9 mm package. These individually calibrated high accuracy sensors are serialized for traceability and provide a typical accuracy of ±2% for relative humidity and ±0.2°C for temperature. They come in a compact 6-pin DFN package, provide a fast response time and have a typical power consumption of only 3.78μW. The sensors are available in both a digital I2C format with configurable addresses as well as an analog version.
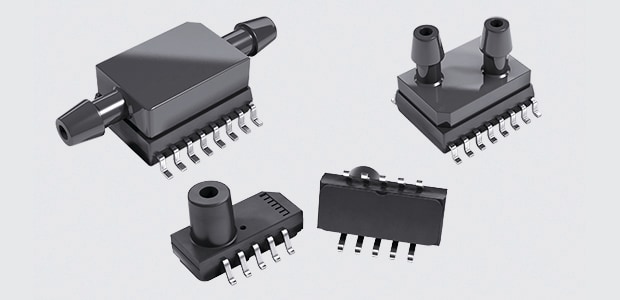
TE also offers low pressure sensors that can be used to monitor and regulate the line pressure that keeps the trachea open. Differential versions of these can be used to monitor/regulate the airflow. These pressure sensors are offered in 16-pin SOIC package that are suitable for surface mounting. TE also offers a wide range of stand-alone temperature sensing technologies that can be used to monitor and control the temperature of the pressurized air in PAP applications or to monitor the room air temperature as part of sleep monitoring applications. Technologies include:
Packages range from a new, fully digital TSYS03 in an ultra-compact XDFN6 package that is only 1.5mm square x 0.38mm with ±0.5°C accuracy from 0°C to 60°C to a wide range of packaged assemblies with a variety of temperature ranges, accuracies and sizes.
Finally, we manufacture a range of board and surface mount anisotropic magnetoresistive (AMR) position sensors that are widely used in motor and fan controls to accurately monitor rotation or linear displacement. Their small size, high accuracy and high reliability allows them to be designed into many compact, high performance home medical products including PAP machines.

CONCLUSION
Sleep medicine has been an expanding discipline during the last few decades. The prevalence of sleep disorders is increasing, and a range of products continue to be developed to monitor and treat sleep disorders. Many new methods for recording sleep and diagnosing sleep disorders have been developed. Sleep disorders are chronic conditions and require continuous treatment and monitoring of therapy success. Cost-efficient technologies for the initial diagnosis and for follow-up monitoring of treatment are important. This is one example of telemedicine technologies meeting the demands of diagnosis and treatment of sleep disorders. Sensors play a critical role in both the monitoring of sleep either in a clinical or home environment as well as in the devices used to treat the most common sleep disorder – sleep apnea.